논문으로 살펴보겠습니다.
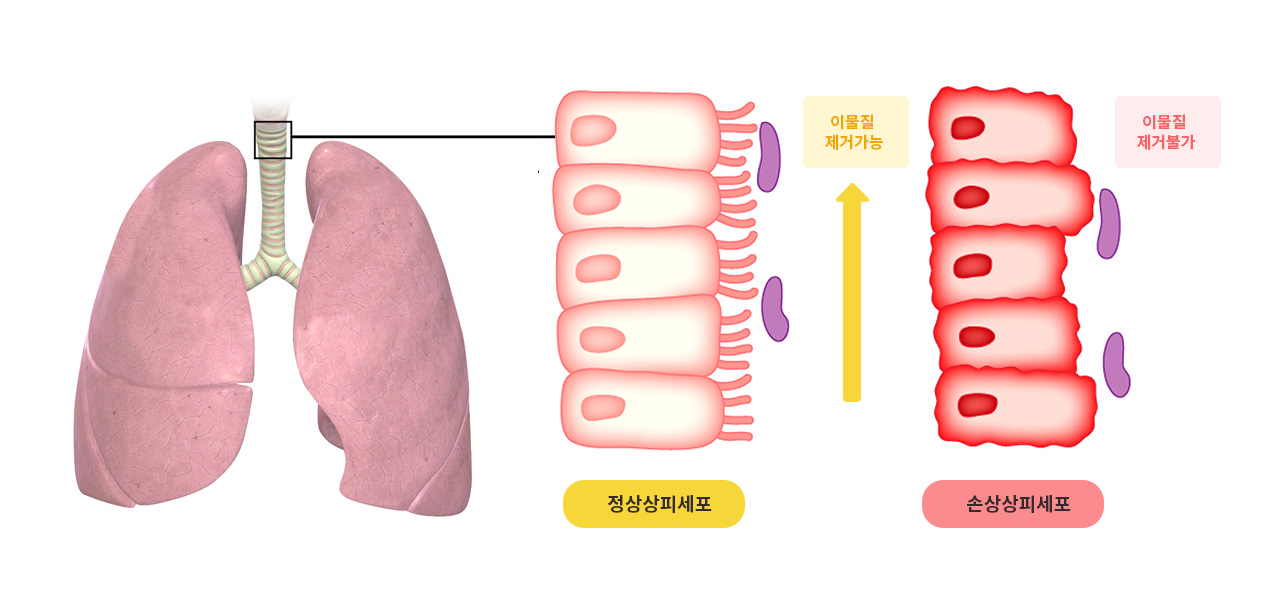
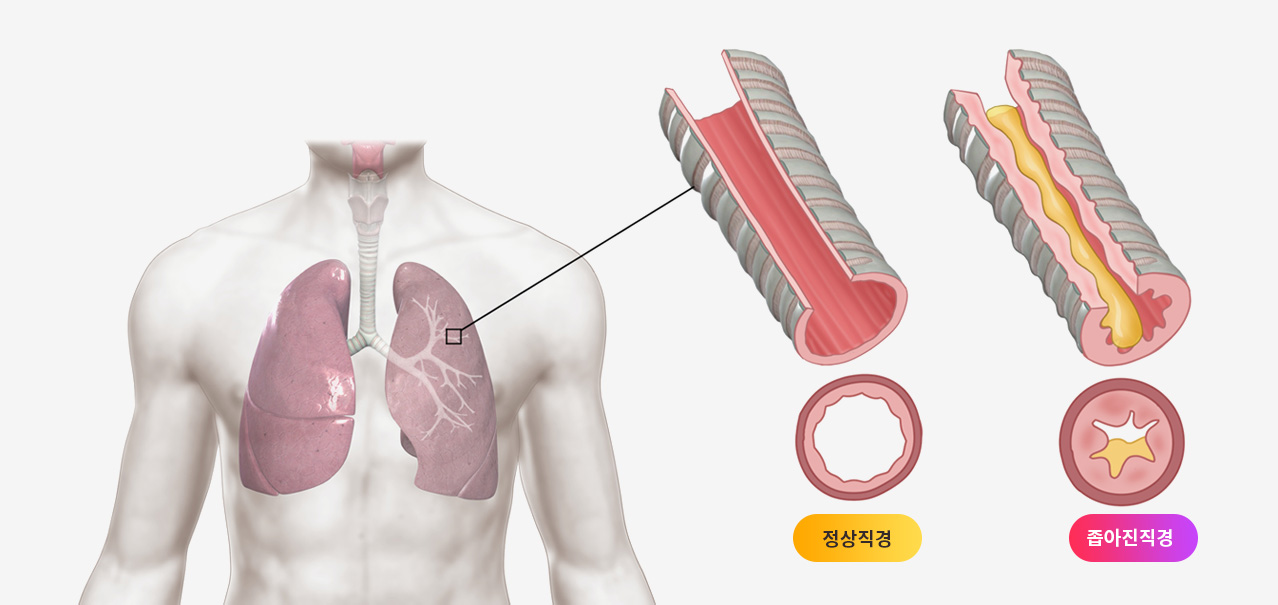
* 한약이 가래를 해결하고 면역 및 폐 환기 기능을 개선하는 효과가 있다는 논문(중국)
Clinical and experimental study on jinshui liujun decoction in treating chronic bronchitis
[Article in Chinese] C Y Zhao 1, Y S Shen, H Meng
Abstract
Objective
To assess the effect of Jinshui Liujun decoction (JSL) in treating chronic bronchitis.
Methods: The effect of JSL on expelling the phlegm and strengthening the body resistance were observed.
Results
JSL was proved to be efficacious in improving immune function of the body and pulmonary ventilatory function (P < 0.01). JSL could not only increase the secretion of rats' trachea mucosa and dilute sputum, but also increase the motion speed of the pigeons' trachea cilia, thus facilitate the removal of sputum. Compared with the normal saline control group, both animal experiments displayed significant statistical difference (P < 0.01), but without significant difference when compared the JSL group with the positive drug Juhong Tanke Ye control group. Conclusion JSL has the effect of resolving phlegm as well as improving human immunological and pulmonary ventilatory functions. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1997 May;17(5):264-6.
* 한약은 장기간의 기침 치료에 안전하고 유용하다는 논문(일본)
Antitussive effect of bakumondoto a fixed kampo medicine (six herbal components) for treatment of post-infectious prolonged cough: controlled clinical pilot study with 19 patients
Kazunori Irifune 1, Hironobu Hamada, Ryoji Ito, Hitoshi Katayama, Akira Watanabe, Aki Kato, Seigo Miyoshi, Naohiko Hamaguchi, Ryo Toyozawa, Sachiko Hamaguchi, Masahiro Abe, Kazutaka Nishimura, Jitsuo Higaki
Abstract
Bakumondoto (TJ-29) is a traditional herbal medicine that has been used in Japan for the treatment of bronchitis, bronchial asthma, and cough. This study investigated the effect of TJ-29 for the treatment of post-infectious prolonged cough. We performed a multicenter randomized controlled trial treating patients without (group A, n=11) or with TJ-29 (group B, n=8) for a total of 2 weeks using a beta 2 stimulant as the basal agent. Efficacy and safety were compared by a cough diary, VAS and sleeping questionnaire. At 4 and 5 days after treatment, the cough score of group B showed significant improvement compared with group A, demonstrating an early antitussive effect. At the assessment 2 weeks after treatment start, both groups showed similar levels of improvement in the cough score. No significant difference was observed in the VAS and the sleeping questionnaire items. In conclusion, oral TJ-29 administration could be useful and safe for the treatment of post-infectious prolonged cough.
Phytomedicine. 2011 Jun 15;18(8-9):630-3. doi:10.1016/j.phymed.2011.02.017. Epub 2011 Apr 22.
* 신뢰할 수 있는 조언과 근거지침에 근거해서 기관지염에 한약 사용을 추천할 거라는 논문(영국)
Herbal medicine for acute bronchitis: A qualitative interview study of patients' and health professionals' views
Dia Soilemezi 1, Geraldine M Leydon 1, Ruiyang Yan 2, Catherine Simpson 3, Margaret Bell 3, Jennifer Bostock 3, Michael Moore 1, Merlin Willcox 4
Abstract
Background: Antibiotics are widely prescribed for acute bronchitis in the UK. Herbal medicine could be used instead to provide symptom relief.
Aim: To explore the views of patients and health professionals on using herbal medicine for acute bronchitis instead of antibiotics.
Design and setting: This was a nested qualitative study, conducted alongside a feasibility randomised clinical trial which ran from July 2018 to May 2019 in 20 GP practices in Wessex, UK.
Method: We conducted telephone semi-structured interviews with patients and with health professionals. The interview data were transcribed and analysed thematically.
Results: Overall, 40 interviews were conducted with 29 patients, six GPs and five nurses. While some patients believed antibiotics are more effective, most were aware of resistance and were keen to try an alternative, including herbal medicine. Several patients believed herbals would be "less intrusive" than antibiotics, whereas a few disliked the taste or experienced side-effects after taking a herbal. Professionals were concerned about potential interactions with conventional medicines. Many patients trusted herbals because of their long history of use, while some did not understand them. Availability of herbals without a prescription enables patients to use them for self-care, but their cost was a barrier for some. Many patients were willing to take a herbal if advised by their GP. Most GPs were happy to recommend a herbal, if endorsed by evidence-based guidelines.
Conclusion: Many patients and health professionals would consider using herbal medicine for acute bronchitis, if based on trustworthy advice and evidence-based guidelines respectively.

















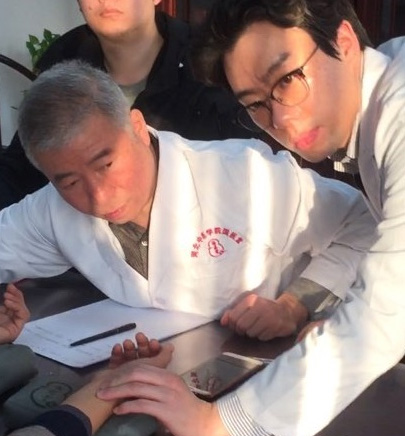 이사무 선생의 진료실에서
이사무 선생의 진료실에서


